Chlamydia

Disclaimer: Not medical or professional advice.
As recently as 30 years ago no one heard about chlamydia: there is simply no data on the incidence until the mid-1980s. So where did it come from and does it have a history?
The history of chlamydia dates back to 1907, when a Czech scientist Stanislav von Provazek set out on an expedition to the island of Java to study syphilis. Provazek conducted an interesting experiment: he infected orangutans with scrapes from the conjunctiva of Indonesians with trachoma. So, a previously unknown microorganism was found, which was named Chlamydozoa. Which in translation from Greek means a cloak wrapped around the shoulder. The researcher associated it with the antique chlamys when he saw the inclusions of microbes "draping" the nucleus of the infected cell.
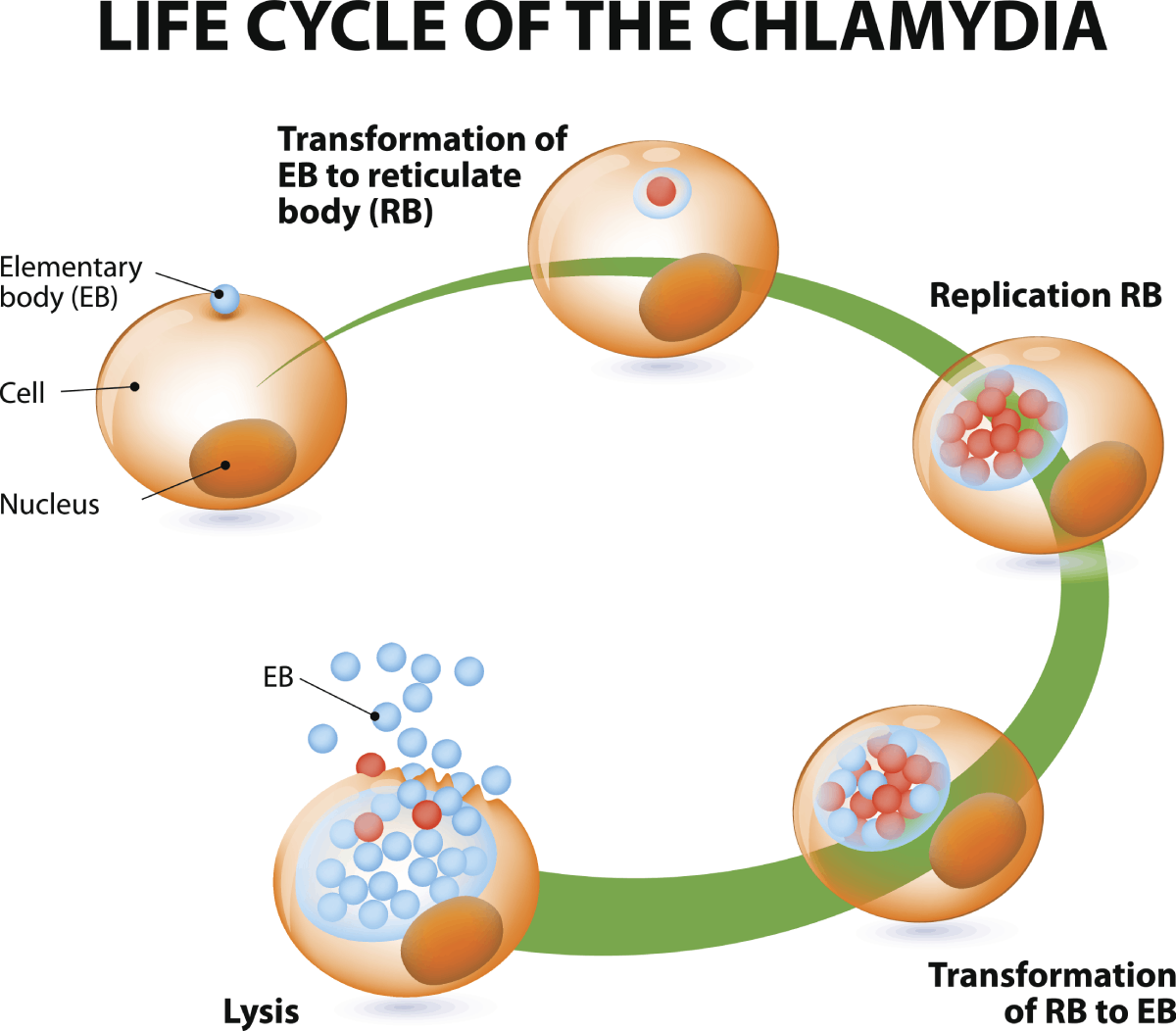
For a very long time, scientists could not understand to whom chlamydia should be attributed — bacteria or viruses. In 1957, the microbe was isolated from the chicken embryo, and in 1963 — from the cell culture. Only then did it finally become clear that Chlamydia trachomatis is a bacterium. But only in the '80-s of the past century the relation between chlamydia infection and inflammatory diseases of urogenital tract was proven...
The medical world had been moving towards this discovery since 1965, when the morbidity of urethritis, which was not associated with either syphilis or gonorrhea, increased sharply. The alarming trend made doctors start looking for a new pathogen. The pathogenic agent was found, but the answer to the question of whether cases of urethritis were caused by chlamydial infection or not remained a mystery. Apparently, no one will ever know from where and when urogenital chlamydia came to us. But it came and is not going to leave. Today, chlamydia is one of the most common sexually transmitted diseases. Every year around the world, an average of 100 million infections are recorded.
How is Chlamydia Transmitted?
Clinical studies show that transmission of chlamydia occurs in 30-50% of cases, even after the first unprotected sexual contact (oral, anal, genital). When detecting chlamydia in a person, it is imperative to check the permanent sexual partner, since the risk of infection with regularly repeated sexual intercourse is almost 100%.
What other Ways Can Chlamydia be Transmitted?
- A profession associated with an increased risk of psittacosis (veterinary medicine, livestock sector, etc.) or the presence of poultry.
- The presence of other genital infections — gonorrhea, syphilis, trichomoniasis.
Chlamydia is not a harmless disease. It is dangerous because of its complications both from the genitourinary system and from other organs - eyes, joints, lungs.
Why Chlamydia is Dangerous for Women.
- Due to its asymptomatic course, chlamydia is rarely detected in the initial stages. The bacteria continue to spread in the body for months or even years. The first symptoms of chlamydia are unpleasant vaginal discharge, painful urination, and fever.
- Inflammation of the pelvic organs. The infection affects the uterus and appendages, causing pain, fever. If the inflammation lasts a long time, adhesions develop — dense fibers from connective tissue.
- Ectopic pregnancy. The fertilized egg gets stuck in the fallopian tube or cannot attach to the mucous membrane because of the synechia and chronic inflammation, caused by chlamydia.
- Infertility. Chronic chlamydia, even without symptoms, can make the fallopian tubes impassable, so pregnancy cannot occur naturally.
- Infections Newborn. If the baby's mother had chlamydia at the time of delivery, bacteria can enter the baby's eyes and cause conjunctivitis or enter the lungs, causing pneumonia.
The Laboratory Diagnosis of Chlamydia
The CDC recommends testing for chlamydia once a year for all sexually active women and men. The examination should be done even if there are no signs of the infection.
There are several methods for diagnosing chlamydia. Since chlamydia live inside the cells, a scrape instead of a smear should be taken. That is, the material sample must contain living cells.
- The most informative and accurate method for determining chlamydia is polymerase chain reaction (PCR). This analysis requires scraping from the urethra or cervical canal, prostate secretions and ejaculate, the first portion of urine, blood, saliva. All body fluids are not required. It all depends on where the inflammatory process is.
- The method of enzyme immunoassay is a study of venous blood for the antibodies to chlamydia. This method is indicative only 5-20 days after the onset of the disease.
- The microbiological method (plating on chlamydia) is necessary to determine the antibiotic to the causative agent of the disease.
In order to be tested for chlamydia, you must adhere to simple rules - to exclude alcohol two days before the analysis. Blood from a vein must be taken on an empty stomach to obtain a more accurate result. For taking scrapes from the genitals and urethra. It is necessary to refrain from sexual intercourse for 1-2 days and not to urinate for at least an hour before taking the material.
Why does Chlamydia Become Chronic?
It is much more difficult to cure chlamydia than to get it. The disease is one of the most concealed of the venereal. Therefore, patients often receive a diagnosis of the chronic form. Information that for many years bacteria inhabited their bodies puts patients into a stupor, the question arises - is chlamydia fully treated? Doctors answer - chlamydia in women (in men) is a curable disease.
In chronic chlamydia, it is really difficult to choose a therapy regimen due to the resistance of bacteria to the active components of many drugs. It may take years from the moment of infection until the disease is detected, during which time a person undergoes antibiotic therapy for other diseases. The concentration of active substances was not enough to destroy chlamydia, and they acquired Immunity to some drugs.
A timely detected disease is much easier to treat. It is enough to take a course of antibiotics and you can forget about the problem. The competence and experience of the doctor are very important in this matter. Illiterate treatment will only make the situation worse.
How do You Prevent Chlamydia?
- Refusal from casual and unprotected sex.
- Timely full examination and treatment with minimal signs of genitourinary infections of the patient and his sexual contacts.
- Annual full preventive examination by a gynecologist or urologist.
Timely diagnosis, treatment and prevention of chlamydia will help to avoid reproductive health disorders and irreversible consequences of the disease. If you have any suspicious symptoms, visit a specialist right away. If you wish, you can be screened for chlamydia and other genital infections anonymously.
7 Myths about Chlamydia
Myth 1. You can catch chlamydia through the toilet seat. Intimate relationships have nothing to do with it.
Many patients report that they got chlamydia because they used someone else's toilet seat. It is not true.
It is almost impossible to get chlamydia in a shared bathroom, even if it is used by a carrier of the infection. Chlamydia is also not spread through the exchange of items such as towels.
The sexual form of chlamydia spreads through unprotected sex of any form. Contamination is also possible if you share sex toys.
Myth 2. Chlamydia will go away on its own, it does not need to be treated.
Some diseases and infections can go away on their own due to the strong immunity of the person. Therefore, it is not surprising that patients ask themselves: does chlamydia go away on its own?
The infection is curable only with antibiotics. Proper therapy usually resolves chlamydia in one to two weeks.
If chlamydia is left untreated, it will not go away on its own, but will cause a number of serious complications. In women, the infection spreads to the uterus and fallopian tubes. And in men - on the prostate gland. Chlamydia can also affect joints, causing reactive arthritis.
Myth 3. Chlamydia can only be transmitted through traditional intimate relationships.
You may have heard that chlamydia cannot be obtained through oral or anal contact, but this is just a myth. An unprotected relationship with the contact of any mucous membranes increases the risk of developing chlamydia. The degree of risk varies depending on gender and presence of contraception.
The only method of contraception that can protect against sexually transmitted diseases is condoms. Other types of contraception - birth control pills and IUDs - do not provide protection against chlamydia and other sexually transmitted infections.
Myth 4. You will know right away if you or your partner gets chlamydia.
Chlamydia is a dangerous disease, but its symptoms do not appear immediately. Therefore, upon infection, it is impossible to guess that a pathological process has begun. And even after a few months, you may not notice anything.
Most women and about half of men with chlamydia have no symptoms at all. This is why it is so important to regularly pass tests for infections.
Myth 5. You are insured against chlamydia if you have already suffered it.
Many infectious diseases occur in the human body only once, as immunity is developed. Unfortunately, this is not the case for chlamydia. Recurrent chlamydial infections are very common.
Myth 6. Chlamydia is nothing serious.
Chlamydia is the most common bacterial sexually transmitted infection in the world.
In 15% of women, chlamydia spreads to the uterus and fallopian tubes, leading to symptomatic pelvic inflammatory disease. In addition, some patients have subclinical inflammation of the upper genital tract, irreversibly damaging the affected tissues.
Myth 7. Chlamydia is not transmitted through a single contact.
There is a myth that chlamydia cannot be obtained as a result of one sexual intercourse. In fact, the infection is easily transmitted after the first time.
If you have had an unprotected intimate relationship, pass a smear and urine analysis. This disease, detected in the early stages, is easily and quickly treated.